Heads-Up: Massive Public-Interest Health Paper About to Land.
New Zealanders have been told that rising rates of diabetes, heart disease, obesity, anxiety, depression, & neurocognitive disorders are complex and best managed one condition at a time.
A forthcoming paper from Physicians and Scientists for Global Responsibility New Zealand (PSGRNZ) directly challenges that framing.
Reclaiming Health: Reversal, Remission & Rewiring is nearing release, and its central message is both confronting and hopeful: much of what we now treat as inevitable chronic disease is driven by shared upstream biological processes, and a significant proportion of this burden is preventable, modifiable, and in many cases reversible.
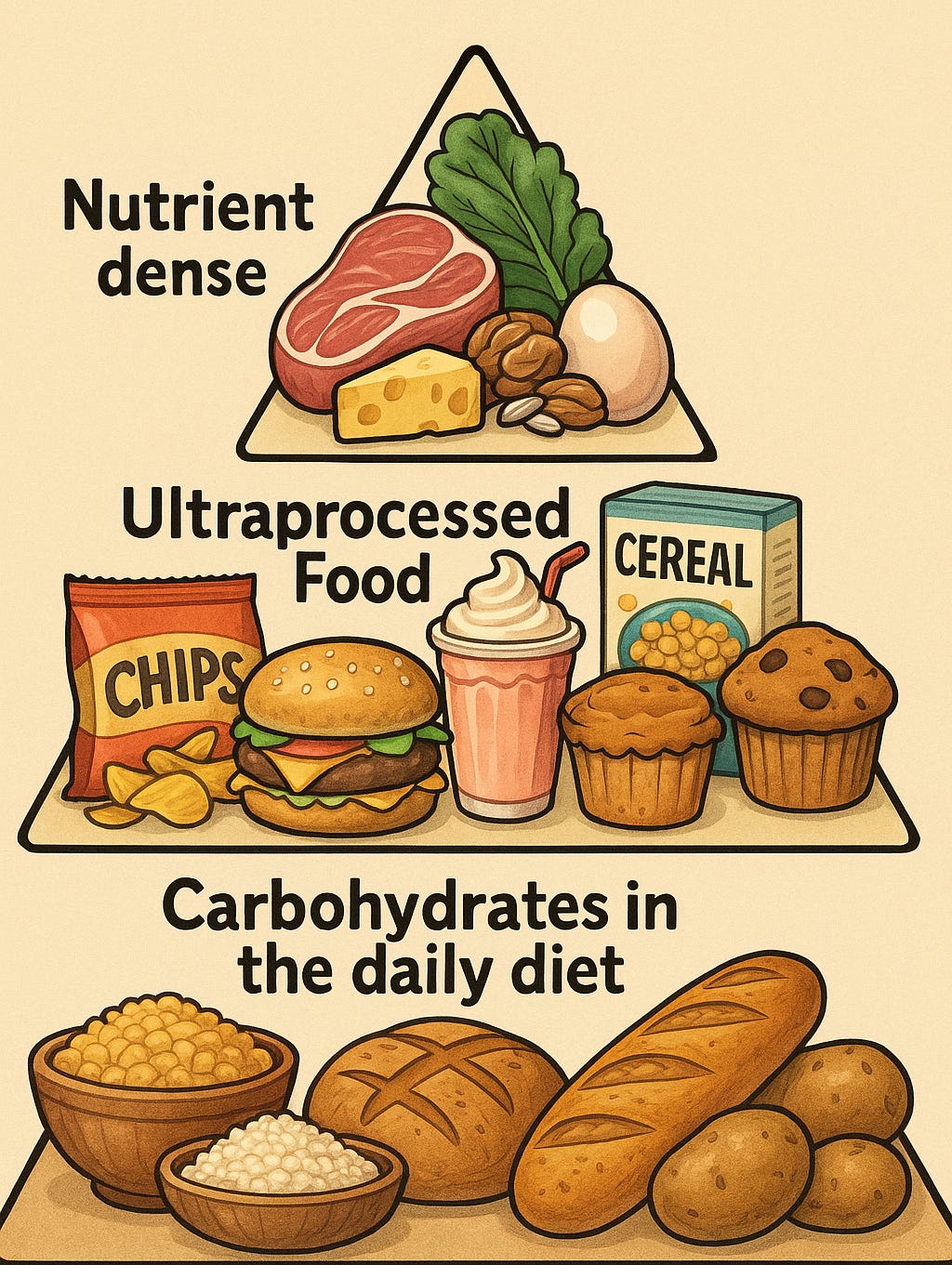
The paper synthesises evidence across metabolic science, nutrition, psychiatry, clinical practice, and population data to show that many of today’s most common physical and mental health conditions are not separate problems, but expressions of the same underlying metabolic disruption. Rather than focusing narrowly on individual diagnoses, it asks a more fundamental question: what happens when policy, guidelines, and institutions drift away from human biology?
What makes this work different is not just its scope, but its timing. The science around insulin resistance, cumulative carbohydrate exposure, food addiction, and micronutrient sufficiency has matured rapidly. At the same time, multimorbidity is appearing earlier in life, medication use is rising, and health systems are under growing fiscal and workforce strain. The gap between what is known and what is formally recommended has become difficult to ignore.
Youtube Short (19/12/2025): Reality Check Radio. “Increasing rates of pre-diabetes, diabetes, cancer, autoimmune...” — Jodie Bruning
Audio interview: Reality Check Radio (RCR). December 19, 2025 Interview with Paul Brennan: Metabolic Crisis, Missed Science. (48:24)
PSGRNZ’s forthcoming paper does not shy away from that gap. It examines how dietary guidance has remained anchored to deficiency prevention rather than optimal metabolic and brain health, how policy frameworks have narrowed what counts as “relevant evidence”, and how individuals are often left without meaningful informed consent about the likely trajectory of metabolic and mental illness once diagnoses such as “prediabetes” or anxiety are applied.
Importantly, the paper is not an abstract critique. It documents real-world examples, from New Zealand and internationally, where diet-first approaches, carbohydrate reduction, improved nutrient density, health coaching, and community support have led to measurable improvements: remission of type 2 diabetes, reductions in prescribing, improved cardiovascular markers, and better mental wellbeing. These outcomes are not framed as miracles or one-size-fits-all solutions, but as signals that the prevailing “manage forever” model is incomplete.
One of the most encouraging aspects of the project has been the response from experts. PSGRNZ has received statements of support from internationally recognised clinicians and researchers, including paediatricians and epidemiologists, who work at the intersection of metabolism, nutrition, mental health and chronic disease. Their contributions do not simply endorse the paper’s conclusions; they reinforce a growing consensus that metabolic health has been under-recognised as a unifying driver of modern disease.
These expert statements will be published alongside the report. Together, they reflect a clinical and academic shift that has been building quietly for years: away from viewing chronic disease as an inevitable by-product of ageing or personal failure, and towards understanding it as a systems problem shaped by food environments, policy choices, and biological stressors.
There is also a strong New Zealand voice in this work. Local clinicians and researchers are contributing evidence and experience from primary care and community settings, where remission and improvement are already being observed. Their perspective matters, because it grounds the science in everyday practice and demonstrates that change is possible within existing health systems when incentives and support are aligned.
A December Reality Check Radio interview with journalist Paul Brennan discussed many of the themes that are explored in the soon-to-be-released paper.
PSGRNZ describes the forthcoming paper as a public-interest intervention rather than an advocacy document. Its aim is not to prescribe a single diet or approach, but to widen the scope of what is considered legitimate, evidence-based, and ethically necessary in health policy and clinical care. This includes recognising food addiction as a real biological challenge, acknowledging individual metabolic variability, and challenges many long-taken-for-granted presumptions.
For readers, clinicians, policymakers, and communities alike, Reclaiming Health is intended as a signal that the conversation is changing. The question is no longer whether chronic metabolic and mental illness will continue to rise, but whether institutions are prepared to respond to what the science is now showing.
The full paper will be released shortly. Based on the content and citations, the breadth of coverage, and the momentum building around it, it is one to watch closely.





Than k you, I look forward to it. So good the conversation is changing to a more holistic model of health
YouTube cancelled everything I wrote after once mentioning covid